What are the similarities and differences between myeloma and AL amyloidosis?
AL amyloidosis (also referred to as light chain amyloidosis) is a rare disease that, similarly to myeloma, arises due to abnormal plasma cells, which are a type of immune cell. These abnormal plasma cells reside in the bone marrow. The most important difference between the two diseases is that in myeloma, the abnormal plasma cells proliferate uncontrollably and cause problems for the bones. Meanwhile, in AL amyloidosis, the pathology is caused by the build-up of misfolded (incorrectly assembled) light chain proteins produced by the abnormal plasma cells, and which deposit in organs and tissues, leading to organ disfunction. In most patients with AL amyloidosis, plasma cells make up less than 20% of the bone marrow. In myeloma, the uncontrollably proliferating plasma cells in the bone marrow can disrupt its normal functioning, producing anaemia, hypercalcemia, renal failure and/or bone lytic lesions (areas where bone has been destroyed, leaving a hole in the bone), as well as plasmacytomas (tumours of plasma cells of bony or soft tissue).
The following table outlines some of the differences between the two conditions:
***********************************************
- Incidence: the number of patients who are diagnosed every year with the disease out of a million people.
- This number indicates the median percentage of abnormal plasma cells in the bone marrow of patients. The median is the value for which half of the observations are larger and half are smaller.
What symptoms are characteristic of myeloma and AL amyloidosis?
The non-specificity of the symptoms is one of the causes of diagnosis delays. These delays are estimated to be on average 163 days for myeloma and 180-441 days for AL amyloidosis, between the first consultation and the diagnosis, after consulting numerous different physicians.
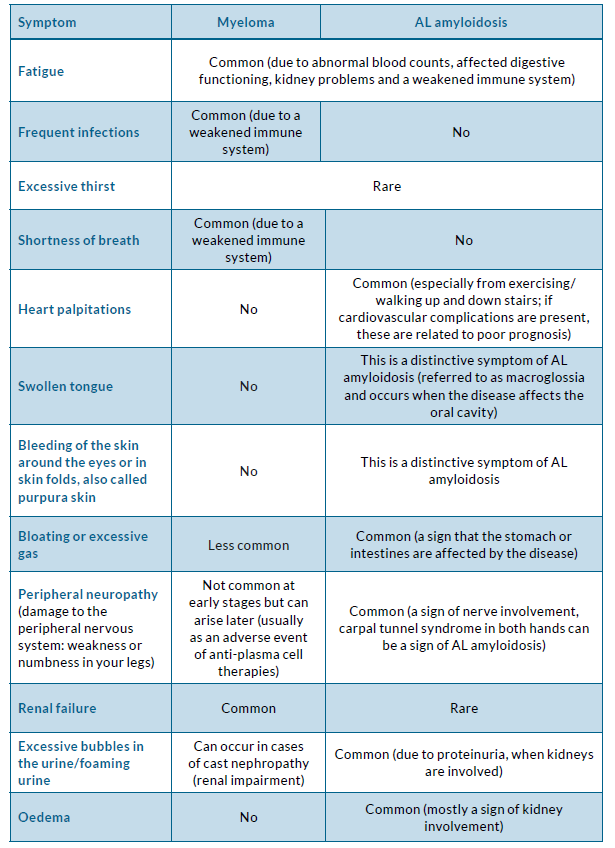
Because of their overlapping pathophysiology, the two diseases have several common symptoms, however, some symptoms are more specific for one of the two illnesses. The following table summarises the symptoms that myeloma and AL amyloidosis patients most regularly experience and indicates which of the two diseases can cause them.
Comparison of myeloma and AL amyloidosis symptoms
Are the two illnesses related to each other?
Yes, both diseases are in the spectrum of plasma cell cancers and are therefore related. This is because both diseases arise due to abnormal plasma cells in the bone marrow. Plasma cells are a type of immune cell that produce antibodies (molecules designed to fight infections). In myeloma, abnormal plasma cells proliferate uncontrollably and produce one type of antibody, known as paraprotein or M-protein, which is made up of heavy and light chains but has no known useful function. In patients with AL amyloidosis, plasma cells do not proliferate uncontrollably, and they produce abnormal, antibody light chains, which misfold and bind together deposition tissues and organs as amyloid fibrils, causing damage and affecting organ function. Unfortunately, to date, there are no treatment options for removing the body of these amyloid deposits. The goal of treatment is to prevent further deposits by stopping the production of these toxic light chains. Notably, there are ongoing clinical trials exploring ways to clear out the amyloid deposits responsible for the organ damage present. If you would like to find out more about these, please see the “Clinical trials” section of MPE’s AL amyloidosis guide.
Can myeloma follow from AL amyloidosis or vice versa?
Approximately 12–15% of myeloma patients will develop amyloidosis at a later stage of their disease, and around 30% of myeloma patients develop subclinical amyloid deposits, which means the amyloidosis is not fully manifested. In both cases, this disease is called myeloma associated amyloidosis and it is treated in the same way as myeloma. It is rare for a patient with AL amyloidosis to develop myeloma.
Effective myeloma treatment is the best option to prevent any exacerbation of your condition. As a result of their shared pathophysiology, treatment of both diseases uses the same procedures and drugs because the goal is to abolish the malignant plasma cell clones. But importantly, the doses and schedule of these drugs can be very different due to the fragility of AL amyloidosis patients who cannot tolerate standard myeloma regimes.
What is the prognosis for AL amyloidosis vs myeloma?
The prognosis of myeloma and AL amyloidosis is affected by many different factors, so it is not possible to predict how long an individual is likely to live. Your prognosis will depend on the exact nature of your disease and on your general health and well-being. For example, smoking and drinking alcohol can have a significant negative impact on your prognostic outlook, while regular light exercise and healthy eating may improve your prognosis. Some other factors such as age can play a role. Usually, younger patients can more safely undergo high intensity treatment and procedures like a stem cell transplant, which can lead to markedly improved prognosis.
For myeloma patients a factor can be your cytogenetic risk. Certain features of the genetic abnormalities in the plasma cells are associated with high-risk disease characteristics in myeloma. For example, part of chromosome 4 has swapped places with chromosome 14 in translocation t(4;14). This abnormality can be found in all or subgroups of myeloma cells and results in high-risk disease characteristics. Other common translocations in myeloma cells include t(14;16), t(6;14), and t(14;20). In general, however, approximately half the people diagnosed with myeloma survive for five years or more. The prognosis of AL amyloidosis is highly dependent on the extent of heart involvement. In patients with severe heart disease, approximately half of patients survive beyond six months. Therefore, early diagnosis is of the upmost importance. Both diseases have benefitted greatly from all the new developments in therapy, especially immune therapy.
What treatment options exist for myeloma and AL amyloidosis?
Since both myeloma and AL amyloidosis are caused by the presence of abnormal plasma cells, the same treatment approaches may benefit both patient groups. For more details, see the MPE myeloma and AL amyloidosis guides.
For both diseases, the choice of treatment will depend on age, general health and wellbeing and, in AL amyloidosis, the stage of the cardiac disease. Patients under the age 65-70 with myeloma in relatively good physical condition will be offered higher doses of drug treatments. This is generally followed by intensive treatment with chemotherapy to eliminate the abnormal plasma cells and stem cells, and a stem cell transplant to replace the killed stem cells inside the body. Older patients (over 70 years), and patients who are less able to tolerate the side effects of intensive treatment (such as those with severe cardiac involvement), are more likely to receive less intense treatment and generally a stem cell transplant is not an option for them. Other types of treatments, such as radiation therapy and surgery, may be needed in specific cases. For example, radiation may be used to treat bone areas affected by myeloma that have not responded to drug treatment and are causing pain. In AL amyloidosis, younger patients are in most cases too vulnerable to undergo high-dose chemotherapy and stem cell transplant, and therefore undergo less intensive schedules.
To date, the only approved therapy specifically for the treatment of AL amyloidosis is the combination of the immunotherapy drug daratumumab and chemotherapy drugs cyclophosphamide and bortezomib with the corticosteroid dexamethasone (Dara-CyBorD). Further effective combinations that your doctor may recommend are bortezomib, the chemotherapy drug melphalan and dexamethasone (BMDex), as well as cyclophosphamide, bortezomib and dexamethasone (CyBorD). The doses of these drugs and schedule of administration are different than used in myeloma although the type of drugs is the same. These schedules can be given in an outpatient clinic.
An autologous stem cell transplant (ASCT) involves the use of your own blood stem cells to replace the killed stem cells by the high-dose chemotherapy given previously. This approach is often effective because it leads to the eradication of the plasma cells for a long time. ASCT can significantly prolong survival, however, only approximately 20% of patients with AL amyloidosis qualify for this, as you
need to be in otherwise good health to safely undergo the procedure. For a stem cell transplant, you have to stay in hospital for several weeks.
Reversal of organ damage, as well as the removal of amyloid deposits that are already present in tissues, is challenging. However, there are some novel drugs in clinical trials that are designed to enable the removal of amyloid deposits (see the section titled “Clinical trials” in MPE’s AL amyloidosis guide).
What are the most common side effects of treatment?
As myeloma and AL amyloidosis are caused by the presence of abnormal plasma cells, the same treatment approaches may benefit both patient populations and consequently, many side effects reported by patients are the same as well. But those with AL amyloidosis experience more side effects such as increased fatigue, heart failure, neuropathy, low blood pressure and oedema.
Here is a list with a summary of these side effects below.
Please also see MPE’s myeloma and AL amyloidosis guides, as these provide tips on how to cope with the treatment side effects you may be experiencing.
- Blood clots
- Low blood counts (which can lead to infections and easy bruising)
- Tingling and numbness in your hands and feet caused by peripheral
neuropathy (damage to the peripheral nervous system) - Constipation
- Nausea and vomiting
- Diarrhoea
- Fatigue
- Weakened immune system (which can lead to frequent infections as your body will not be able to fight infections efficiently)
- Hair loss
- Dizziness, feeling light-headed
- Excessive thirst
- Dysphagia (difficulty swallowing), mouth or throat sores
- Oedema
- Low blood pressure
Where can I turn to for support and more information on AL amyloidosis?
If you are finding it difficult to cope and your mental health is declining, consult your doctor, as in most healthcare settings, it may be possible to receive counselling. This kind of support may be reimbursed by the health care system in some countries and your doctor will be able to give you information on this. Alternatively, you can reach out to a patient organisation or other voluntary service. If you need support with practical matters, such as help around the house, home help or hospice services may be available. Palliative care services (specialised medical care for people living with a serious illness, which is focused on providing relief from the symptoms and stress of the illness) may also be accessible to you, so make sure you ask about this as well. If you are looking for more information, there are several useful resources available on the MPE website (for example, our AL amyloidosis guide and factsheets). Also follow MPE on our social media channels (Facebook, Twitter, YouTube) for regular updates related to myeloma and AL amyloidosis. It might be a good idea to join a local patient/advocacy group that represents amyloidosis patients (if one exists in your country). It can be very helpful to form connections with others who are struggling with the same illness as you. Furthermore, you will gain access to valuable information about the disease and treatment options, which healthcare professionals to turn to, self-caring and career suggestions etc.
The group might host social events as well, and attending these can be a motivating, informative and positive experience. Examples of such groups are:
- Austria: Leben mit Amyloidose.
- France: Association Française contre l’Amylose.
- Germany: Amyloidose Selbshilfegruppe.
- Israel: Amyloidosis Israel.
- Italy: Associazione Italiana contro leucemi limfomi e mieloma (AIL).
- Macedonia: Association for help and support of patients and their caregivers with hematological diseases (HEMA).
- Netherlands: Stichting Amyloïdose Nederland (SAN).
- Norway: Blodkreftforeningenn.
- Slovakia: Slovak Myeloma Society (SMyS).
- Slovenia: Association of Patients with Blood Diseases Slovenia.
- Spain: Asociación Española de Amiloidosis (AMILO).
- United Kingdom: Myeloma UK.
Alternatively, you may consider reaching out to an umbrella organisation (like MPE) or other non-profit organisations that represent AL amyloidosis patients for support and information. Examples of such organisations are:
References:
- AL Amyloidosis Foundation (2023). AL – Amyloidosis Foundation.
- Minnema, M. C. et al. Differences and Similarities in Treatment Paradigms and Goals between AL Amyloidosis and Multiple Myeloma. Hemato 2021, Vol. 2, Pages 680-691 2, 680–691 (2021).
- Myeloma UK. AL amyloidosis.
- City of Hope Cancer Center (2022). Multiple myeloma symptoms.
- Myeloma Patients Europe (2023). About Myeloma: What are the symptoms?
- Bahlis, N. J. & Lazarus, H. M. Multiple myeloma-associated AL amyloidosis: is a distinctive therapeutic approach warranted? Bone Marrow Transplantation 2006 38:1 38, 7–15 (2006).
- American Cancer Society (2018). What Is Multiple Myeloma?
- MyMyelomaTeam (2021). Myeloma Lifestyle Changes: Drinking and Smoking Habits.
- Abdallah, N. et al. Cytogenetic abnormalities in multiple myeloma: association with disease characteristics and treatment response. Blood Cancer J 10, (2020).
- WebMD (2023). Multiple Myeloma Stages and Prognosis.
- American Cancer Society (2018). Radiation therapy for Multiple Myeloma.
- Wani, Z., Harkawat, D. K. & Sharma, M. Amyloidosis and Anesthesia. Anesthesia, Essays and Researches 11, 233 (2017).
- Orphanet (2021). AL amyloidosis.